Organ transplant pioneer Dr. Joseph E. Murray died November 26, 2012, in Boston. The New York Times reports that Murray, “who opened a new era of medicine [in 1954] with the first successful human organ transplant, . . . was awarded the [1990] Nobel Prize in Physiology or Medicine.”
Organ transplant pioneer Dr. Joseph E. Murray died November 26, 2012, in Boston. The New York Times reports that Murray, “who opened a new era of medicine [in 1954] with the first successful human organ transplant, . . . was awarded the [1990] Nobel Prize in Physiology or Medicine.”
As director of the Surgical Research Laboratory at Harvard Medical School and at Peter Bent Brigham Hospital in Boston, which became Brigham and Women’s, Dr. Murray was a leader in the study of transplant techniques, the mechanisms of organ rejection and the use of drugs to thwart it.
Among other procedures, he performed kidney transplants involving more than two dozen pairs of identical twins. He performed the first successful transplant to a nonidentical recipient, in 1959, and the first using a cadaver kidney, in 1962. And he trained doctors who became leaders in transplantation around the world.
Murray’s pioneering progress was not easy. The New Jersey Star-Ledger’s Jim Namiotka noted that Murray’s success was “the product of grueling trial-and-error using animals and cadavers, then volunteer patients. . . .” In addition to the tremendous scientific challenges he faced, Murray also had to confront religious accusations that he was “playing God.” Murray, though himself a religious man, dismissed those charges and forged ahead with his work. Since Murray’s 1954 breakthrough, “more than 600,000 transplants have occurred worldwide.”
Yet, despite the tremendous benefits of modern transplant technology owing to heroic pioneers such as Dr. Murray, many people cannot get the treatment they need. Namiotka notes that while “Nearly 20,000 transplant surgeries took place in the United States during the first eight months of this year,” there are still “more than 116,000 patients . . . on waiting lists.” This bottleneck is due largely to the primitive altruist ethics—itself rooted in religious dogma—that scorns material compensation and profit. Consequently, as Craig Biddle notes, many thousands of people suffer and die needlessly every year because of a shortage of organ donors.
It’s long past time that our ethics caught up with our medical progress. We must recognize the morality—indeed, the nobility—of profiting from providing a value to another in a mutually beneficial, voluntary trade. We must call for the abolition of laws restricting or banning donor compensation and profit, thus opening up free trade in a free market for human organs. As the time-tested laws of economics dictate, that would go a long way toward giving those 116,000 patients a shot at an organ—and life.
Could there be a better way to honor Dr. Joseph E. Murray’s incredible legacy?
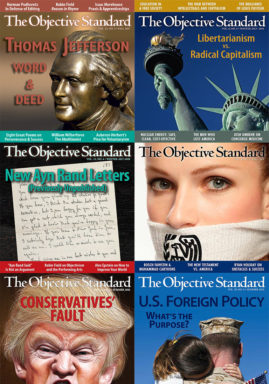
Like this post? Join our mailing list to receive our weekly digest. And for in-depth commentary from an Objectivist perspective, subscribe to our quarterly journal, The Objective Standard.
Related:
- Altruism: the Morality of Suffering and Death (Exhibit 347R: Organ Donation)
- Obama’s “Cruel Disregard” for the Sick—and the Well
- Institute for Justice Wins Victory in Bone-Marrow Compensation Case
Image: iStockPhoto
![[TEST] The Objective Standard](https://test.theobjectivestandard.com/wp-content/uploads/2017/10/logo.png)